The case for vulnerable plaque.
Every 40 seconds across the United States, another person experiences a heart attack.
According to the Centers for Disease Control and Prevention, myocardial infarctions (heart attacks) happen in 805,000 people each year in the US. It is the first heart attack for more than 600,000 people.
These heart attacks contribute to cardiovascular disease’s top billing as the leading cause of death in the US and globally. It is also the leading burden of disease in terms of its impact over a lifespan.
But while contemporary diagnostic tools for heart disease are effective at coronary assessment through artery narrowing (stenosis) and hardening (calcification), they do not address the underlying cause of most heart attacks. This means a large proportion of our population may not see heart attacks coming nor take actions for preventative care.
The majority of heart attacks occur when fatty deposits in the coronary arteries – known as high-risk plaques or vulnerable plaque – rupture, move and block the blood vessel.
This blockage reduces the blood and oxygen available for the heart muscle’s optimal function and can lead to permanent muscle damage. In cases of severe blockage, this can be fatal.
It is the rupture of the vulnerable plaque that is the actual cause of the blockage and the heart attack. Yet, it is not routinely reported in cardiac imaging and diagnostics.
Cutting edge research is demonstrating the critical role vulnerable plaques play in major adverse cardiovascular events. Their presence in the arteries can be a predictor of major cardiac events, such as heart attack. So why don’t we look for them in medical imaging?
Vulnerable plaques are very difficult to detect using non-invasive contemporary techniques. Traditionally, detection of vulnerable plaques has only been achievable using specialised intravascular ultrasound and an invasive coronary angiogram. An angiogram involves inserting an imaging probe into the coronary artery to be able to visualise it. Because it is invasive, coronary angiograms carry the risk of puncture and discomfort.
Coronary computed tomography angiography (CCTA) is now the class 1A recommendation for evaluation of symptomatic patients with known coronary artery disease (CAD). Due to the recent update to the American College of Cardiology guidelines, the use of non-invasive CCTA to check for the presence of coronary artery plaques and narrowing of the arteries is expected to grow.
Yet to report on vulnerable plaque, a highly skilled radiologist and cardiologist would have to assess those images to locate and assess the disease. This would be effective, but it is a time-consuming and very challenging undertaking, even for expert clinicians. For this reason, vulnerable plaque is rarely reported. This can lead to CAD being under-diagnosed, non-personalised care and over utilisation of coronary angiograms, an invasive procedure that should be reserved for when extensive diagnostic coronary artery disease has already been detected.
This is where AI and deep learning can improve the detection and diagnosis of coronary artery disease – and highlight the presence of critical vulnerable plaques. Deep learning algorithms are trained to detect discrepancies down to the pixel level.
Vulnerable plaques have an identifiable composition, made up of lipids and inflammatory cells surrounded by thin vessels. Through deep learning, an AI solution can recognise and flag the vulnerable plaques.
Artrya has access to more than 50,000 CCTA scans with many of these used to train, test and validate the AI algorithms.
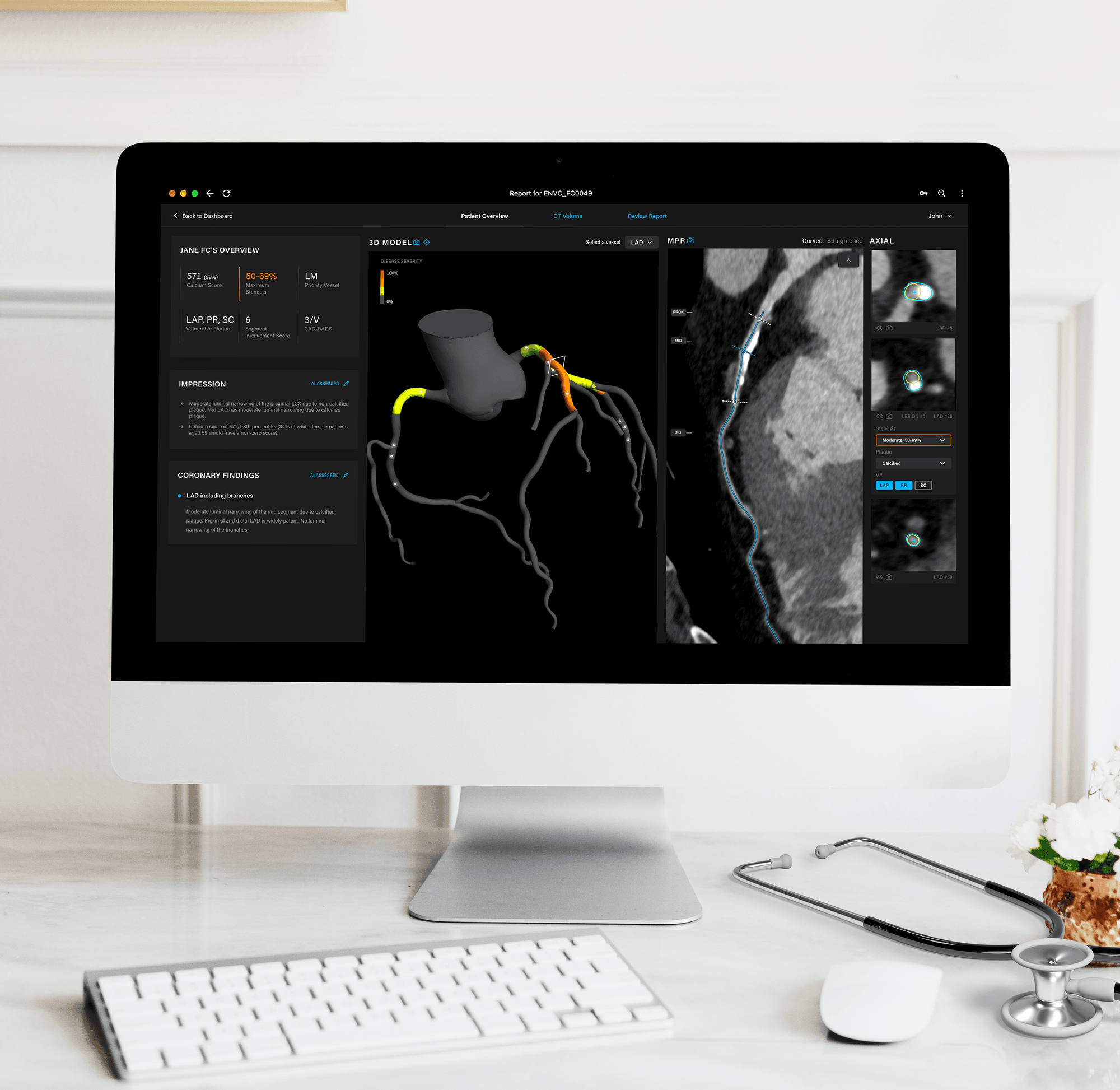
The Artrya Salix software solution can detect and report stenosis, calcification and, importantly, the presence of vulnerable plaque, to create a comprehensive picture of CAD and at-risk patients.
The solution can detect vulnerable plaque with an accuracy greater than 70 per cent. Due to the nature of detecting vulnerable plaque without AI-assistance, it is reported that expert readers have an accuracy of 65 per cent1 which demonstrates the difficulty. Importantly, with a 15-minute turnaround time, using Artrya Salix makes it possible to deliver a report including vulnerable plaque assessment within mainstream radiology workflows without excessive cost, time or resource utilisation. Delivering this timely report to clinicians is a game-changer in the diagnosis workflow of coronary artery disease.
Vulnerable plaque and its detection are key areas of medical research. As a diagnostic solution, assessing the presence of vulnerable plaque will allow clinicians to present a clear picture of cardiac risk to their patients.
In turn, this will empower patients to take control of their cardiovascular health and make steps to decrease their risk factors through lifestyle changes and medical management. This includes stopping smoking, eating a healthy diet and reducing stress levels.
Without a transformative change in the trajectory of heart disease, it is on track to cost the American healthcare system more than $1 trillion in less than 15 years.
We want a future where clinicians are enabled to detect and diagnose cardiac health efficiently and quickly. This will facilitate patients to take the steps needed to shift the dial on their own health and act for prevention. Accurate coronary health information is critical to saving healthcare systems, clinicians and ultimately – human lives. That’s what we’re providing – a new way to see heart disease.
(1) Kolossváry M, Karády J, Kikuchi Y, Ivanov A, Schlett CL, Lu MT, Foldyna B, Merkely B, Aerts HJ, Hoffmann U, Maurovich-Horvat P. Radiomics versus Visual and Histogram-based Assessment to Identify Atheromatous Lesions at Coronary CT Angiography: An ex Vivo Study. Radiology. 2019 Oct;293(1):89-96. doi: 10.1148/radiol.2019190407. Epub 2019 Aug 6. PMID: 31385755; PMCID: PMC6776230.